About Iopofosine I 131
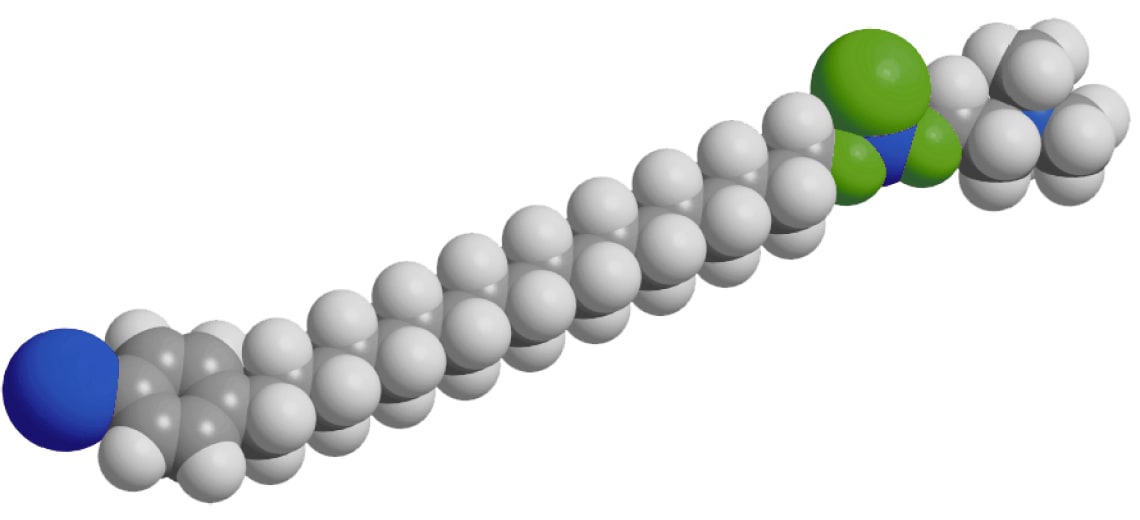
Iopofosine I-131 is Cellectar’s lead investigational phospholipid drug conjugate (PDC) radiotherapeutic, designed to deliver iodine-131 directly to tumor cells while minimizing exposure to healthy tissue.
Iopofosine I-131 has been evaluated in the completed CLOVER-WaM Phase 2 pivotal study for patients with relapsed or refractory Waldenström macroglobulinemia (WM) and continues to be studied in a Phase 2b trial in relapsed or refractory multiple myeloma and CNS lymphoma, as well as the CLOVER-2 Phase 1b study in pediatric patients with high-grade glioma.